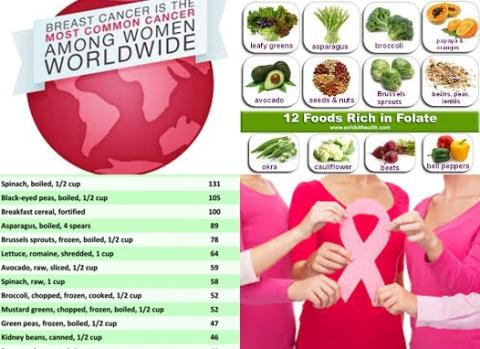
Low-fat diet reduces recurrence of breast cancer
Objectives:
Even though many studies have examined the possible effect of low-fat diet on breast cancer survival, the relationship remains unclear. Therefore, this review article has been conducted.
Does low-fat diet reduce risk of recurrence of breast cancer?
Study design:
This review article included 2 randomized controlled trials (RCTs) and 1 large multi-center prospective cohort study with 9,966 breast cancer patients.
Results and conclusions:
The investigators found post-diagnostic low-fat diet significantly reduced risk of recurrence of breast cancer by 23% [HR = 0.77, 95% CI = 0.63 to 0.94, p = 0.009] and all cause mortality of breast cancer by 17% [HR = 0.83, 95% CI = 0.69 to 1.00, p = 0.05].
The investigators concluded post-diagnostic low-fat diet reduces risk of recurrence of breast cancer. However, more trials of the relationship between low-fat diet and all-cause mortality of breast cancer are still needed.
Original title:
Effect of low-fat diet on breast cancer survival: a meta-analysis by Xing MY, Xu SZ and Shen P.
Link:
https://pubmed.ncbi.nlm.nih.gov/24606431/
Additional information of El Mondo:
Find more information/studies on fat consumption and breast cancer right here.
A low-fat diet is a diet with maximum 30 En% fat and maximum 7 En% saturated fat.
30 En% fat means that the amounts of fat contribute 30% to the total calories (kcal) of the diet.
If the diet contains 2000 kcal, 66.7 grams of fat contribute 30% to this 2000 kcal.
1 gram of fat gives 9 kcal. Thus, 66.7 grams of fat provide 600 kcal and 600 kcal is 30% of 2000 kcal.
The most easy way to follow a diet a diet with maximum 30 En% fat and maximum 7 En% saturated fat is to choose only meals/products with maximum 30 En% fat and maximum 7 En% saturated fat. Check here which products contain maximum 30 En% fat and maximum 7 En% saturated fat.
However, the most practical way to follow a diet with maximum 30 En% fat and maximum 7 En% saturated fat is, all meals/products that you eat on a daily basis should contain on average maximum 30 En% fat and maximum 7 En% saturated fat.
To do this, use the 7-points nutritional profile app to see whether your daily diet contains maximum 30 En% fat and maximum 7 En% saturated fat.