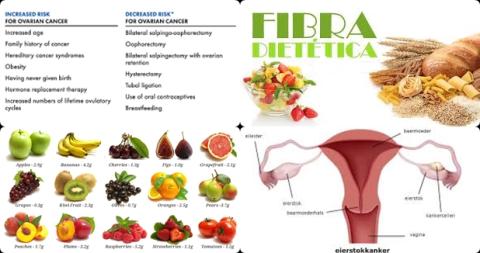
10g dietary fiber intake per day may reduce ovarian cancer risk
Objectives:
Epidemiological studies regarding the association between dietary fiber intake and ovarian cancer risk are still inconsistent. Therefore, this review article has been conducted.
Does dietary fiber intake reduce ovarian cancer risk?
Study design:
This review article included 10 case-control studies and 3 cohort studies, with a total of 5,777 ovarian cancer cases and 142,189 participants.
All the included studies provided RRs that were adjusted for energy intake and most provided RRs that were adjusted for age, oral contraceptive use, menopausal status and parity.
All the original studies measured dietary intakes using a food-frequency questionnaire. NOS scores ranged from 6 to 8 and 7 studies were considered high quality.
Funnel plot shapes demonstrated a symmetrical distribution and no evidence of publication bias was detected by the Egger’s regression test [p = 0.73].
Results and conclusions:
The investigators found for the highest vs. the lowest category of dietary fiber intake a significantly reduced risk of 22% [pooled multivariable RR = 0.78, 95% CI = 0.70 to 0.88, I2 = 4.20%, p = 0.40] for ovarian cancer.
The investigators found a significantly reduced risk of 12% [summarized RR = 0.88, 95% CI = 0.82 to 0.93, I2 = 7.3%, p = 0.38] for ovarian cancer per 10 g/day increase of dietary fiber intake.
The investigators found there was no evidence for a nonlinear association between dietary fiber intake and ovarian cancer risk [p for nonlinearity = 0.83].
The investigators found in subgroup analysis a significantly reduced risk of 23% [pooled RR = 0.77, 95% CI = 0.66 to 0.90] for ovarian cancer in case-control studies. However, the reduced risk was not significant in cohort studies [pooled RR = 0.84, 95% CI = 0.65 to 1.10].
The investigators found sensitivity analysis showed that none of the studies influenced the combined results substantially, with a range from 0.77 [95% CI = 0.68 to 0.87] to 0.81 [95% CI = 0.71 to 0.91].
The investigators concluded that 10g dietary fiber intake per day may reduce the risk of ovarian cancer with 12%. May reduce because the reduced risk was not significant in cohort studies.
Original title:
Dietary fiber intake and reduced risk of ovarian cancer: a meta-analysis by Zheng B, Shen H, […], Qin Y.
Link:
https://nutritionj.biomedcentral.com/articles/10.1186/s12937-018-0407-1
Additional information of El Mondo:
Find more information/studies on meta-analysis/cohort studies, fiber intake and cancer right here.