Higher vitamin B2 and B6 dietary intake decreases ER-/PR- breast cancer
Objectives:
Epidemiologic studies focusing on the association between 1-carbon metabolism-related vitamins (ie, folate, vitamin B6, vitamin B2, vitamin B12) and breast cancer risk have reported inconsistent findings. Therefore, this review article (meta-analysis) has been conducted.
Does higher dietary intake of folate (folic acid), vitamin B2, B6 or B12 reduce breast cancer risk?
Study design:
This review article included 27 studies (case-control and cohort studies) with a total of 49,707 cases (persons with breast cancer) among 1,274,060 individuals.
Results and conclusions:
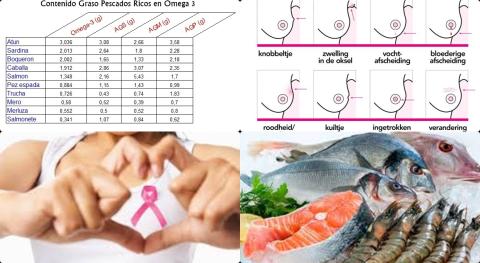
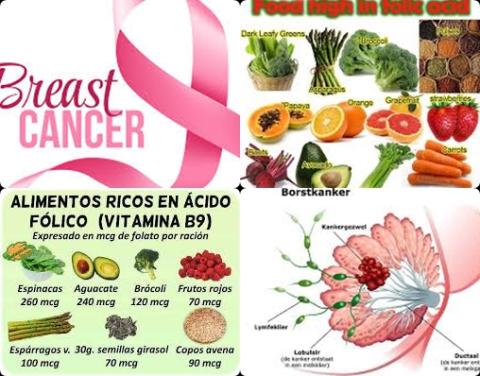
The investigators found for the highest folate dietary intake compared with the lowest, a significantly reduced risk of 7% [pooled relative risk = 0.93, 95% CI = 0.88 to 0.99, p = 0.018] for breast cancer.
The investigators found for the highest vitamin B6 dietary intake compared with the lowest, a significantly reduced risk of 6% [pooled relative risk = 0.94, 95% CI = 0.89 to 1.00, p = 0.037] for breast cancer.
The investigators found for the highest vitamin B2 dietary intake compared with the lowest, a significantly reduced risk of 10% [pooled relative risk = 0.90, 95% CI = 0.82 to 0.99, p = 0.026] for breast cancer.
The investigators found no significant association between vitamin B12 and breast cancer risk [RR = 0.99, 95% CI = 0.94 to 1.04, p = 0.604].
The investigators found folate and vitamin B6 dietary intake significantly decreased the risk of estrogen receptor-negative (ER-)/progesterone receptor-negative (PR-) breast cancer but not ER+/PR+ breast cancer.
The investigators found an increment of 100 μg/d folate dietary intake corresponded to a 7% [RR = 0.93, 95% CI = 0.89 to 0.98, p = 9.007] deceased risk of ER-/PR- breast cancer.
The investigators concluded both higher folate, vitamin B2 and B6 dietary intake decreases risk of breast cancer, especially ER-/PR- breast cancer.
Original title:
Association Between One-carbon Metabolism-related Vitamins and Risk of Breast Cancer: A Systematic Review and Meta-analysis of Prospective Studies by Zeng J, Gu Y, […], Chang H.
Link:
https://www.ncbi.nlm.nih.gov/pubmed/32241696
Additional information of El Mondo:
Find more information/studies on folate, vitamin B2 and B6 intake and breast cancer right here.
If breast cancer cells have estrogen receptors, the cancer is called ER-positive breast cancer. If breast cancer cells have progesterone receptors, the cancer is called PR-positive breast cancer. If the cells do not have either of these 2 receptors, the cancer is called ER/PR-negative.