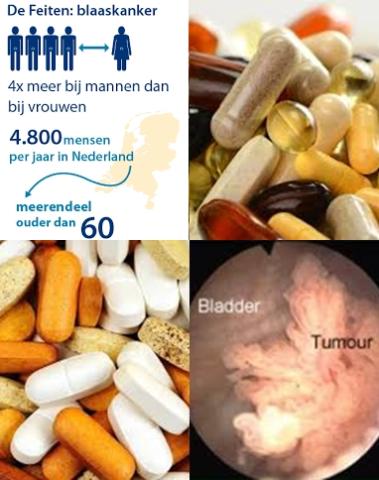
Vitamin and antioxidant supplements have no overall preventive effect against bladder cancer
Objectives:
Recently, several randomized controlled trials (RCTs) reported the association between the use of vitamin or antioxidant supplements and the risk of bladder cancer. However, those findings remain inconsistent and some studies even reported that vitamin and antioxidant supplements increased the risk of bladder cancer. Therefore, this review article (meta-analysis) has been conducted.
Is there an association between the use of vitamin or antioxidant supplements and the risk of bladder cancer?
Study design:
This review article included 14 RCTs with a total of 147,383 participants, which involved 89,972 in the supplement group and 57,411 in the control group.
The supplementation and follow-up periods ranged between 1 and 13 years.
The types of vitamin and antioxidant supplements were as follows: vitamin A, vitamin B6, vitamin C, vitamin D, vitamin E, beta-carotene, folic acid and selenium.
The dosage regimens in individual trials were as follows: vitamin A (200 mg or 25,000, 36,000 or 40,000 IU daily), vitamin B6 (25 or 100 mg daily), vitamin C (2,000 mg daily), vitamin D (1,600 IU daily), vitamin E (50 mg or 400 IU daily), beta-carotene (20 or 30 mg daily; 50 mg alternate day; 75 mg daily for 3-month cycles), folic acid (1.6 mg daily) and selenium (200 μg daily).
Publication bias was not observed [Begg's funnel plot, symmetrical and Egger's test, p for bias = 0.378].
Results and conclusions:
The investigators found in fixed-effect meta-analysis of all 14 trials that vitamin or antioxidant supplementation was not associated with the risk of bladder cancer [RR = 1.04, 95% CI = 0.92-1.17, I2 = 39.7%].
The investigators found regarding types of supplements, any type of vitamin and antioxidant supplements had no beneficial effect on the risk of bladder cancer:
-vitamin A [RR = 0.86, 95% CI = 0.65-1.13, I2 = 61.7%, n = 5];
-vitamin B6 [RR = 0.77, 95% CI = 0.49-1.20, I2 = 78.8%, n = 3];
-vitamin C [RR = 0.74, 95% CI = 0.36-1.54, I2 = 88.8%, n = 2];
-vitamin D [RR = 1.05, 95% CI = 0.85-1.29, n = 1];
-vitamin E [RR = 0.91, 95% CI = 0.69-1.19, I2 = 60.9%, n = 6];
-beta-carotene [RR = 1.19, 95% CI = 0.96-1.46, I2 = 0.0%, n = 6];
-folate [RR = 1.05, 95% CI = 0.85-1.29, n = 1] and
-selenium [RR = 1.09, 95% CI = 0.81-1.46, I2 = 0.0%, n = 2].
The investigators found overall, there was no significant effect of vitamin and antioxidant supplements in the subgroup meta-analyses by various factors such as dose of supplements, type of cancer prevention, methodological quality, duration of treatment, provider of supplements, type of control and number of participants.
However, the risk of bladder cancer was marginally increased in trials with the use of beta-carotene alone [RR = 1.44, 95% CI = 1.00-2.09, I2 = 0.0%, n = 3].
The investigators concluded that vitamin and antioxidant supplements have no overall preventive effect against bladder cancer. Instead, subgroup meta-analyses showed that beta-carotene supplementation marginally increased the risk of bladder cancer. Even though further large, high-quality trials are required to confirm these associations, the effects (either beneficial or harmful) of vitamin or antioxidant supplements on bladder cancer should not be overemphasized.
Original title:
Effects of Vitamin and Antioxidant Supplements in Prevention of Bladder Cancer: a Meta-Analysis of Randomized Controlled Trials by Park SJ, Myung SK, […], Lee YJ.
Link:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5334161/
Additional information of El Mondo:
Find more information/studies on vitamins, selenium, beta-carotene, antioxidants and cancer right here.