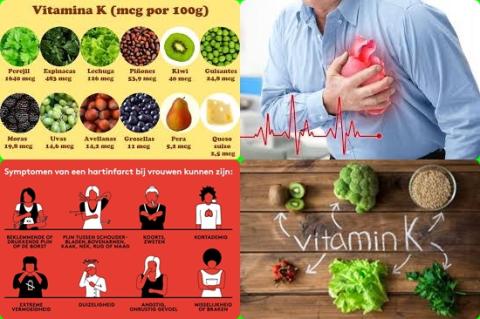
Higher dietary vitamin K consumption reduces risk of cardiovascular disease
Objectives:
Does vitamin K reduce risk of cardiovascular disease (CVD) events and mortality?
Study design:
This review article included 21 articles with 222,592 participants.
Results and conclusions:
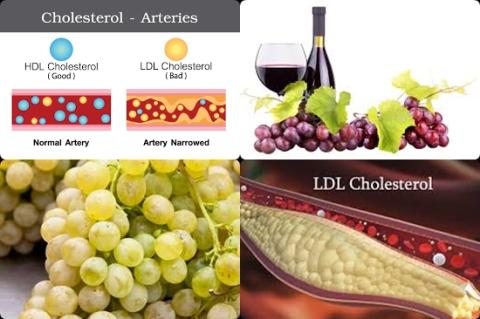
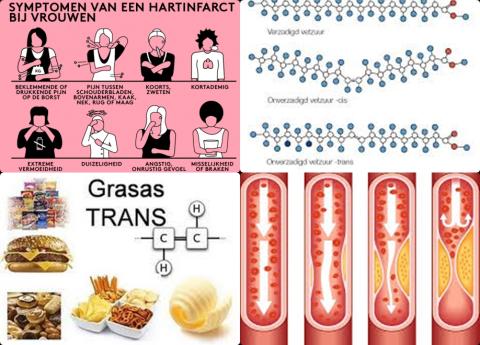
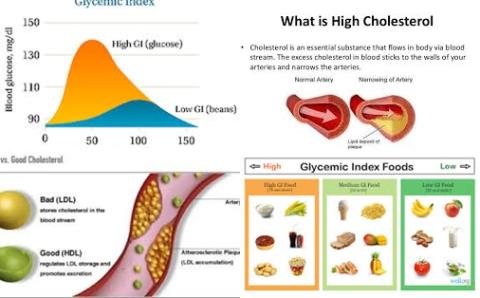
The investigators found dietary phylloquinone (vitamin K1) intake significantly reduced risk of total cardiovascular disease with 8% [pooled HR = 0.92, 95% CI = 0.84 to 0.99, I2 = 0%, 4 studies].
Significant means that there is an association with a 95% confidence.
The investigators found dietary menaquinone (vitamin K2) intake significantly reduced risk of total cardiovascular disease with 30% [pooled HR = 0.70, 95% CI = 0.53 to 0.93, I2 = 32.1%, 2 studies].
Significant because HR of 1 was not found in the 95% CI of 0.53 to 0.93. HR of 1 means no risk/association.
The investigators found no significant association between dietary vitamin K and all-cause mortality, cardiovascular disease mortality or stroke.
The investigators found elevated plasma desphospho-uncarboxylated MGP (dp-ucMGP), a marker of vitamin K deficiency, was associated with an increased risk of 84% [HR = 1.84, 95% CI = 1.48 to 2.28, I2 = 16.8%, 5 studies] for all-cause mortality.
The investigators found elevated plasma desphospho-uncarboxylated MGP (dp-ucMGP), a marker of vitamin K deficiency, was associated with an increased risk of 96% [HR = 1.96, 95% CI = 1.47 to 2.61, I2 = 0%, 2 studies] for cardiovascular disease mortality.
The investigators found no significant association between circulating total osteocalcin and all-cause mortality or total cardiovascular disease.
The investigators concluded higher dietary vitamin K consumption reduces risk of cardiovascular disease and higher plasma dp-ucMGP concentration, but not total circulating osteocalcin, increases risk of all-cause and cardiovascular disease mortality. However, causal relations cannot be established because of limited number of available studies and larger prospective studies and randomized clinical trials are needed to validate these findings.
Original title:
Association of vitamin K with cardiovascular events and all-cause mortality: a systematic review and meta-analysis by Chen HG, Sheng LT, […], Pan A.
Link:
https://www.ncbi.nlm.nih.gov/pubmed/31119401
Additional information of El Mondo:
Find more information/studies on vitamin K, significantly/review article and cardiovascular disease right here.
100 grams of fresh parsley provide 548 micrograms (548 mcg) of vitamin K1 or 4.5 days.