Objectives:
Is there a causal relationship between drinking green tea and improving risk factors of cardiovascular disease, like cholesterol, fasting blood sugar, blood pressure, HbA1c, HOMA-IR?
Study design:
This review article included 55 RCTs with 63 effect sizes with 2,487 participants in the green tea group and 2,387 in the placebo group (group without green tea).
The participants’ mean age ranged between 18 and 68.7 years and the period of intervention ranged between 2 to 48 weeks.
Some of the studies enrolled only males or females and some of them included both genders.
TC, LDL, HDL, FBS, HbA1c and DBP-related evidence had moderate quality due to the serious inconsistency reasons. Additionally, it was shown that evidence regarding TG, fasting insulin, SBP and CRP had low quality due to serious imprecision and inconsistency reasons. The evidence relating to HOMA-IR was also downgraded to very low quality because of the serious inconsistency, imprecision and publication bias.
Results and conclusions:
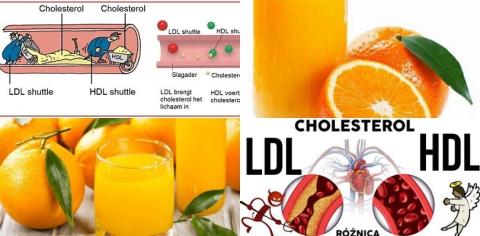
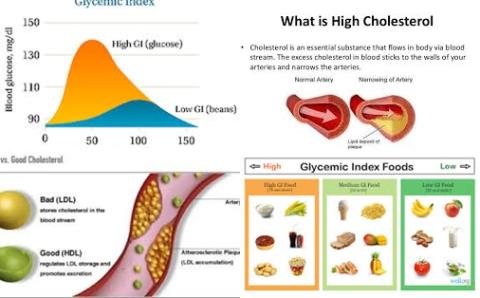
The investigators found green tea supplementation significantly reduced total cholesterol levels (TC) [WMD = -7.62, 95% CI = -10.51 to -4.73, p ≤ 0.001, I2 = 90.9%].
This significantly reduced effect was also found if females or both males and females were included, the dosage of supplementation was less than 1,000 mg/d, the baseline BMI was between 25-29.9 kg/m2 and the baseline value of TC was more than 200 mg/dL.
The investigators found green tea supplementation significantly reduced LDL cholesterol levels (LDL-C) [WMD = -5.80, 95% CI = -8.30 to -3.30, p ≤ 0.001, I2 = 90.5%].
This significantly reduced effect was also found if males or both males and females were included, the baseline BMI was between 25-29.9 kg/m2 and participants were not affected by T2DM.
The investigators found green tea supplementation significantly reduced fasting blood sugar levels (FBS) [WMD = -1.67, 95% CI = -2.58 to -0.75, p ≤ 0.001, I2 = 72.2%].
This significantly reduced effect was also found when the baseline BMI of participants was between 25-29.9 kg/m2, female or both male and female were included, the duration of intervention was more than 12 weeks, the dosage of supplementation was less than 1,000 mg/d and baseline values of FBS were less than 100 mg/dL.
The investigators found green tea supplementation significantly reduced HbA1c levels [WMD = -0.15, 95% CI = -0.26 to -0.04, p = 0.008, I2 = 71.3%].
This significantly reduced effect was also found if the duration of intervention was ≤ 12 weeks, the dosage of supplementation was ≥ 1,000 mg/d, baseline values of HbA1c were less than 6.5%, male or both genders were involved and the baseline value of BMI was ≥ 30 kg/m2.
The investigators found green tea supplementation significantly reduced diastolic blood pressure (DBP) [WMD = -0.87, 95% CI = -1.45 to -0.29, p = 0.003, I2 = 92.4%].
This significantly reduced effect was also found if the duration of intervention was ≤ 12 weeks, the dosage of supplementation was less than 1,000 mg/d, baseline values of DBP were more than 80 mmHg and the baseline value of BMI was ≥ 30 kg/m2.
The investigators found green tea supplementation significantly increased HDL cholesterol levels (HDL-C) [WMD = 1.85, 95% CI = 0.87 to 2.84, p = 0.010, I2 = 94.4%].
This significantly increased effect was also found if females were included, the baseline BMI was lower more than 30 kg/m2, there was no past medical history of T2DM, the duration of intervention was more than 12 weeks, the dosage of supplementation was less than 1,000 mg/d and baseline values of HDL were more than 50 mg/dL.
The investigators found sensitivity analysis showed no significant difference in results with removing one single study for all considered cardiovascular risk factors including lipid profiles, glycemic indices, SBP and DBP and CRP.
The investigators concluded drinking ≤1,000 mg/d green tea may causally improve risk factors of cardiovascular disease. May improve because the RCTs are of low quality.
Original title:
The effects of green tea supplementation on cardiovascular risk factors: A systematic review and meta-analysis by Zamani M, Kelishadi MR, […], Asbaghi O.
Link:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9871939/
Additional information of El Mondo:
Find more information/studies on green tea, lowering blood pressure and cardiovascular diseases right here.