≥75 mg/day isoflavones reduce BMI
Objectives:
Has flavonoid supplementation potential against obesity?
Study design:
This review article included 58 RCTs.
Analysis endpoints were calculated as the mean difference between baseline and post-treatment.
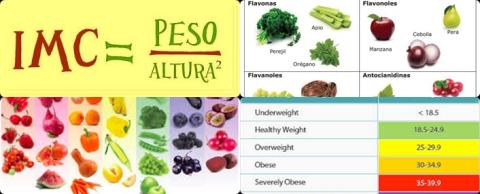
Flavonoids were in subclasses of flavanols, flavonols, isoflavones, flavanones, anthocyanins and proanthocyanidins. They were mostly in the form of supplements and dosages varying from 40 to 1300 mg/day.
Results and conclusions:
The investigators found among flavonoid subclasses, flavanols showed potential for decreasing BMI, in the overall population [MD = -0.28 kg/m2, p = 0.04, n = 21] and in the subgroups of Asians [MD = -0.42 kg/m2, p = 0.046, n = 13], ages 50 years [MD = -0.50 kg/m2, p = 0.008, n = 14], BMI ≥25 kg/m2 [MD = -0.30 kg/m2, p = 0.049, n = 15] and at doses ≥500 mg/day [MD = -0.36 kg/m2, p = 0.049, n = 12].
The investigators found among flavonoid subclasses, isoflavones also significantly decreased BMI of non-Asian populations [MD = -0.26 kg/m2, p = 0.035, n = 13] and doses ≥75 mg/day [MD = -0.34 kg/m2, p = 0.027, n = 8].
The investigators found in the overall assessment, flavanols also significantly decreased waist circumference [MD = -0.60 cm, p = 0.02, n = 18] but had no significant effect on body fat percentage.
The investigators found the available trials did not reveal significant effects from flavonols, flavanones and anthocyanins on the specified anthropometric measures.
The investigators concluded that flavanols, particularly ≥500 mg/day and isoflavones, particularly ≥75 mg/day have potential against obesity.
Original title:
Flavanols are potential anti-obesity agents, a systematic review and meta-analysis of controlled clinical trials by Akhlaghi M, Ghobadi S, […], Mohammadian F.
Link:
https://www.ncbi.nlm.nih.gov/pubmed/29759310
Additional information of El Mondo:
Find more information/studies on flavonoids and overweight right here.