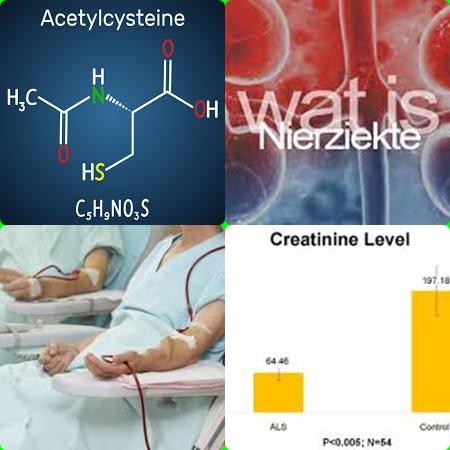
Cardiovascular reserve is improved after kidney-transplantation
Objectives:
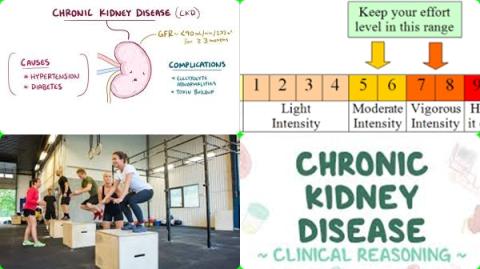
Patients with kidney failure often present with reduced cardiovascular functional reserve and exercise tolerance. Previous studies on cardiorespiratory fitness examined with cardiopulmonary-exercise-testing (CPET) in kidney-transplant-recipients (KTR) had variable results. Therefore, this review article has been conducted.
Does cardiovascular functional reserve improve after kidney-transplantation?
Study design:
This review article included 8 studies with 461 participants.
Results and conclusions:
The investigators found kidney-transplant-recipients had significantly higher oxygen consumption at peak/max exercise (VO2 peak/VO2 max) compared to patients with kidney failure [SMD = 0.70, 95% CI = 0.31 to 1.10, I2 = 70%, p = 0.002].
The investigators found, in subgroup analyses, similar differences were evident among 7 studies comparing kidney-transplant-recipients and hemodialysis patients [SMD = 0.64, 95% CI = 0.16 to 1.12, I2 = 65%, p = 0.009] and 2 studies comparing kidney-transplant-recipients with peritoneal dialysis subjects [SMD = 1.14, 95% CI = 0.19 to 2.09, I2 = 50%, p = 0.16].
The investigators found across 4 studies with relevant data, oxygen consumption during peak/max exercise showed significant improvement after kidney-transplantation compared to pre-transplantation values [WMD = 2.43, 95% CI = 0.01 to 4.85, I2 = 68%, p = 0.02].
The investigators concluded kidney-transplant-recipients exhibit higher cardiovascular functional reserve during cardiopulmonary-exercise-testing compared to patients with kidney failure. Cardiovascular reserve is also improved after kidney-transplantation in relation to pre-surgery levels.
Original title:
Cardiorespiratory fitness in kidney transplant recipients compared to patients with kidney failure: a systematic review and meta-analysis by Theodorakopoulou MP, Boutou AK, […], Sarafidis P.
Link:
https://pubmed.ncbi.nlm.nih.gov/34170572/
Additional information of El Mondo:
Find here more information/studies about review article/significant and kidney disease.
Cardiac reserve or cardiovascular reserve refers to the difference between the rate at which the heart pumps blood and its maximum capacity for pumping blood at any given time. A measurement of the cardiovascular reserve may be a health indicator for some medical conditions, like patients with kidney failure.